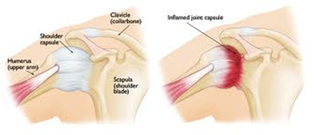
The shoulder joint is surrounded by a strong elastic tissue called the capsule. When this becomes inflamed, it leads to the condition known as frozen shoulder, or adhesive capsulitis. This is a very common disorder (problem) and will affect around 1 in 20 of us at some time in our lives. The cause is not fully understood, it more common in females. It is more likely in those who have had a shoulder injury or shoulder surgery, diabetes or Dupuytren’s disease.
Signs and Symptoms
Pain in the shoulder is usually the first symptom. This is often worse at night and disturbs sleep. Patients describe the pain as occurring, ‘Within the shoulder and going down the arm’. Stiffness in the join soon follows and arm movements become painful: particularly internal rotation (reaching behind the back) and external rotation (turning the palm away from the body). Many people mention pain and difficulty in dressing and overtime develop abnormal movements to cope with this.
These symptoms may gradually improve over a period of 2-5 years (average 30 months). However, studies have suggested 20% of patients still have symptoms beyond 5 years.
Diagnosis
Often the diagnosis is confidently be made following a detailed examination of your arm and shoulder. However, an X-ray and an ultrasound may be required to rule out other shoulder conditions.
Initial Treatment
In some cases, a frozen shoulder can be treated adequately with regular anti-inflammatory medication to ease the pain and allow physiotherapy to begin – it is important to maintain as much movement as possible as the inflammation settles.
Further Treatment
If you have particularly severe symptoms, further treatment options include:
• Hydrodilatation – During this very effective procedure, a combination of saline (salt water), local anaesthetic and steroid are injected into the shoulder joint under X-ray control. Although performed in an operating theatre, there is no need for a general anaesthetic and it is performed as a day-case. If necessary, it can be repeated should symptoms return. After hydrodilatation, you must avoid driving for 24 hours or until shoulder is comfortable.
Hydrodialtion needs to be combined with physiotherapy, but allows more effective physiotherapy to assisit recovery.
Please see images of before and after hydrodilatation:
Before: Restricted movement and pain on shoulder movement
10 mins after and show almost immediately less pain and improved movement
1 week afterwards
2 weeks afterwards
• Arthroscopic Release – This operation is advised for the small number of patients whose symptoms remain severe despite anti-inflammatories, physiotherapy and hydrodilatation. During the arthroscopy (keyhole surgery), the whole shoulder joint is examined, tight areas within the shoulder are released and any bands of scar tissue are removed. Following this operation, patients immediately notice an improved range of shoulder movements, which is then maintained by physiotherapy.